It’s Here! CMS Released the CY 2022 MPFS Final Rule
CY 2022 MPFS Final Rule
Date: 11|04|2021 Approx. 5 min. read
Author: Brianna Plencner, CPC, CPMA Senior Consultant & Manager, Practice Development, HCCI
It’s November and the Centers for Medicare and Medicaid Services (CMS) released the annual Medicare Physician Fee Schedule (MPFS) final rule which outlines what policy and payment impacts healthcare professionals can expect for their services. Here is the CMS fact sheet on the CY 2022 Final Rule.
So, what do home-based professionals and practices need to know?
Let us start with the not-so-great news:
Conversion Factor:
- CMS confirmed the CY 2022 conversion factor is $33.59, a decrease of $1.30 from the CY 2021 MPFS conversion factor of $34.89. This means that we can expect a decrease in fee-for-service reimbursement for our Evaluation & Management (E/M) home and domiciliary CPT codes. CMS is required by law to make changes to account for the budget neutrality adjustment as well as account for the expiration of the temporary 3.75% increase to the conversion factor we benefited from this year because of the Consolidated Appropriations Act, 2021. There is a silver lining, CMS stated they are engaged in an ongoing review of payment for E/M visit code sets. There has been continued advocacy to call attention to the need for positive payment adjustments to the home setting and we are hopeful we may see CMS respond in 2023.
Now let us focus on the positive impacts of the CY 2022 MPFS:
Expanded Telehealth Access for Mental Health:
Right now, and as long as the Public Health Emergency (PHE) declaration remains in effect (which currently will remain in place until at least 01/16/22 with the potential to be extended again) we can continue using the current telehealth and waiver flexibilities.
CMS’s final policy for next year, whenever the PHE ends, will be as follows:
- The home will be an approved originating site and geographic restrictions were eliminated for telehealth services furnished for the purposes of diagnosis, evaluation, or treatment of a mental health disorder. (This was possible because of legislation changes) We would need additional legislation passed to allow the home to be an approved originating site and remove geographic restrictions for Medicare telehealth services for other populations.
- CMS is limiting the use of an audio-only interactive telecommunications system to mental health services furnished by practitioners who have the capability to furnish two-way, audio/video communications, but where the beneficiary is not capable of, or does not consent to, the use of two-way, audio/video technology. A modifier will be required to identify these services.
- Additionally, CMS finalized that certain services added to the Medicare telehealth services list will remain on the list through December 31, 2023.
Increased Reimbursement for Chronic Care Management (CCM) Services:
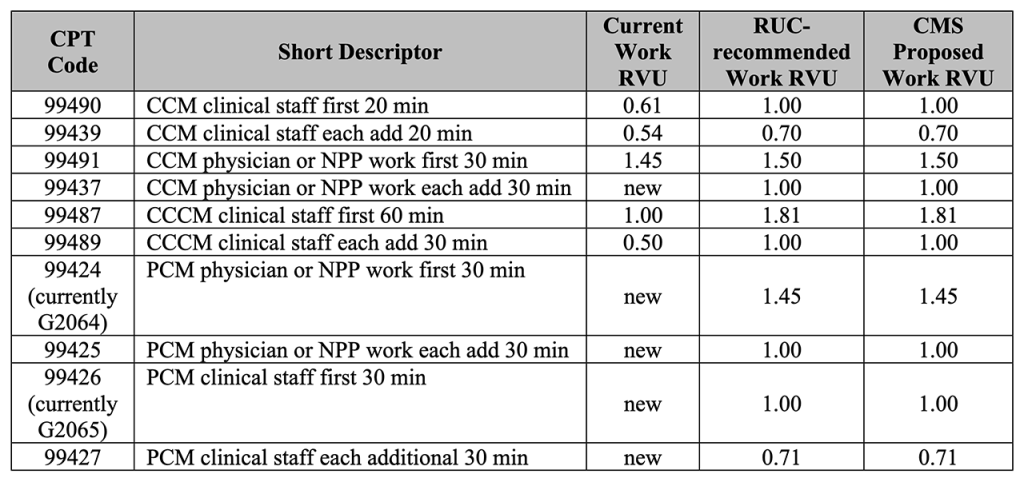
- CMS finalized their policy to increase the wRVU for CCM and Principal Care Management (PCM) services. This offers increased reimbursement for CCM and PCM services in 2022 which offers practices a way to maximize their revenue and offset the loss of decreased reimbursement for our E/M services. Refer to the table below included in the final rule for wRVU changes.
CY 2022 CCM/CCCM/PCM Values
Physician Assistants (PAs) Expanded Scope of Practice:
- Medicare will make direct payment to PAs for professional services furnished under Part B beginning January 1, 2022. Starting January 1, 2022, PAs can bill Medicare directly for their services and reassign payment for their services.
Vaccine Administration Services:
- CMS will pay $30 per dose for the administration of the influenza, pneumococcal and hepatitis B virus vaccines.
- CMS will maintain the current payment rate of $40 per dose for the administration of the COVID-19 vaccines through the end of the calendar year in which the ongoing PHE ends. Effective January 1 of the year following the year in which the PHE ends, the payment rate for COVID-19 vaccine administration will be set at a rate to align with the payment rate for the administration of other Part B preventive vaccines.
- CMS will continue the additional payment of $35.50 for COVID-19 vaccine administration in the home under certain circumstances through the end of the calendar year in which the PHE ends.
Medicare Shared Savings Program (MSSP) & MIPS (Merit Based Incentive Payment System):
- CMS finalized revisions to the repayment mechanism arrangement policy to reduce by 50 percent the existing methodology for determining the repayment mechanism amount.
- CMS finalized a longer transition for Accountable Care Organizations (ACOs) to prepare for reporting electronic clinical quality measures/Merit-based Incentive Payment System clinical quality measures (eCQM/MIPS CQM) under the Alternative Payment Model (APM) Performance Pathway (APP), by extending the availability of the CMS Web Interface collection type for an additional three years, through performance year (PY) 2024.
- Transition to MIPS Value Pathways (MVPs) will not occur until the 2023 performance year.
- The 7 MVPs for the 2023 performance year are: Rheumatology, Stroke Care and Prevention, Heart Disease, Chronic Disease Management, Emergency Medicine, Lower Extremity Joint Repair, and Anesthesia.
- CMS finalized policies that reduce burden and streamline the Shared Savings Program application process.
Spilt or Shared E/M Visits in a Facility Setting:
- CMS finalized their definition and policy for split (or shared) E/M services performed by a Physician and Advance Practice Provider (e.g., Nurse Practitioner or Physician Assistant) in the same group performed in a facility setting (this applies to Skilled Nursing Facility services). The visit is billed by the physician or practitioner who provides the substantive portion of the visit. For 2022, the substantive portion can be history, physical exam, medical decision-making, or more than half of the total time.
- Split (or shared) visits can now be reported for new as well as established patients, and initial and subsequent visits, as well as prolonged services. Further, a modifier is required on the claim to identify these services to inform policy and help ensure program integrity.
For More Information:
The HCCI team is analyzing the CY 2022 MPFS final rule and will provide further information during our upcoming HCCIntelligence webinar:
2022 Coding & Policy Impacts: What Home-Based Providers and Practices need to know!
Wednesday, December 15, 4pm – 5pm