Like Mother, Like Son: An HBPC Physician Shares His Personal Story

Dr. Christopher Paredes
Date: 11|17|2022
At the 2022 American Academy of Home Care Medicine (AAHCM) Annual Meeting last month, James Warda, HCCI’s Vice President of External Affairs and Business Development, presented Driving Practice Growth through Marketing, Media Relations, and Your Community. The course taught participants how to promote their practices to community stakeholders and media outlets through marketing.
“One of the exercises I do in my presentation is to ask the participants to tell their story to the person next to them and then ask the person what stood out to them,” Warda said. “More than an ice breaker, it’s an exercise that makes people think about what sets them apart as well as what they mean to their patients, and their caregivers and families.” After the session, Dr. Christopher Paredes of Northwell Health Physician Partners, shared his personal story with Warda of how he got involved with house calls and why serving the underserved is his personal mission
HCCInsights asked Dr. Paredes to elaborate on his journey into the world of home-based primary care (HBPC) once more to share it with an even larger audience.
HCCInsights: How did you first become involved with HBPC?
Dr. Paredes: I grew up in Queens, New York. My mother (Dr. Tessie T. Paredes – pictured) was and is a solo internal medicine physician in Brooklyn, and my father was a retired colonel. As a teenager, I always wanted to borrow the car, and my mom said, “If you want to borrow the car, you’ll have to drive me to see my patients.” So, I began driving her to these homes where I would usually see a frail, older person come to the door, and they always seemed happy to see my mother.
As time went on, my mom planted some seeds, like maybe one day I could help people through medicine, but I was thinking more about going into finance or trading, the glamorous consulting jobs. Anyway, I finished high school and was trying to decide what was next when my mother was diagnosed with stage three ovarian cancer.

Dr. Tessie T. Paredes
HCCInsights: Did your mother’s diagnosis influence your plans?
Dr. Paredes: It was devastating to find out that our role model, the pillar of our family, our matriarch, was facing this horrible disease. I couldn’t focus, I just wanted to be there for her, and the only degree course that offered the flexibility I needed was psychology. As a psychology major, I learned about behavior at the same time my mom was dealing with surgery and chemotherapy. Amazingly, she never stopped. She paid attention to how her body reacted to the chemotherapy, then scheduled her patients and clinic hours accordingly. She was devoted to serving her patients and the community. There were obvious signs of her illness—her wig, for instance, was a big change from her normal style. But she always carried on with a smile.
The year went by along with her treatment, and we finally got the good news that she was in remission. Faith was a big part of our lives as a Filipino family, and I really felt God had given my mother back to us. To repay God and give thanks, I decided to be like my mom, follow in her footsteps, and serve underserved people by practicing medicine. That’s when I completed the science courses required for medical school and then went to Ross University School of Medicine.
HCCInsights: What sparked your interest in geriatric medicine?
Dr. Paredes: During my residency at Brooklyn Hospital, we saw a lot of older, frail geriatric patients, and I found it easy to form relationships with that age group, probably because I was raised in a culture of respect for our elders. I pursued a geriatric medicine fellowship at Albert Einstein College of Medicine/Montefiore Medical Center and had an opportunity to do home visits. That’s when I saw just how many people are forgotten in their homes—people who were ill and needed care. Long story short, when I finished the fellowship, I applied to work there and was hired to serve patients in the Bronx community, mainly low-income individuals in the inner-city who were really in need.
HCCInsights: How is caring for elderly homebound patients different from providing care in a clinical setting?
Dr. Paredes: Home-based care is different because the home is the patient’s domain, they’re in charge, and it is an honor to be in their home, a privilege. And then it’s all about developing the relationship. I have many stories about how home-based primary care has helped my patients in their most vulnerable times, and it’s not just patients who benefit—it also helps caregivers and family members understand the conditions and the disease trajectories. Because “evidence-based” isn’t evidence-best for everyone. You have to listen, see what the patient can tolerate, and tailor care to the individual by giving them choices and helping them understand what’s happening. Once you empower people, they become more involved in their own care and what they want in life and their medical management. It’s a team approach…like it is in any good relationship.
For example, I once had a patient in Co-op City which is a cooperative housing development in the Bronx. “Mr. W” was an artist with a lot of serious medical conditions and a strong mistrust of the healthcare system and doctors in general. When I first arrived at his apartment, I was amazed by how beautifully his artwork was displayed—there were photographs, sketches, and sculptures, it almost looked like a museum. I spoke with him at length, we went through all his medical conditions, and then he told me it was the first time he felt like he was being treated like a human being.
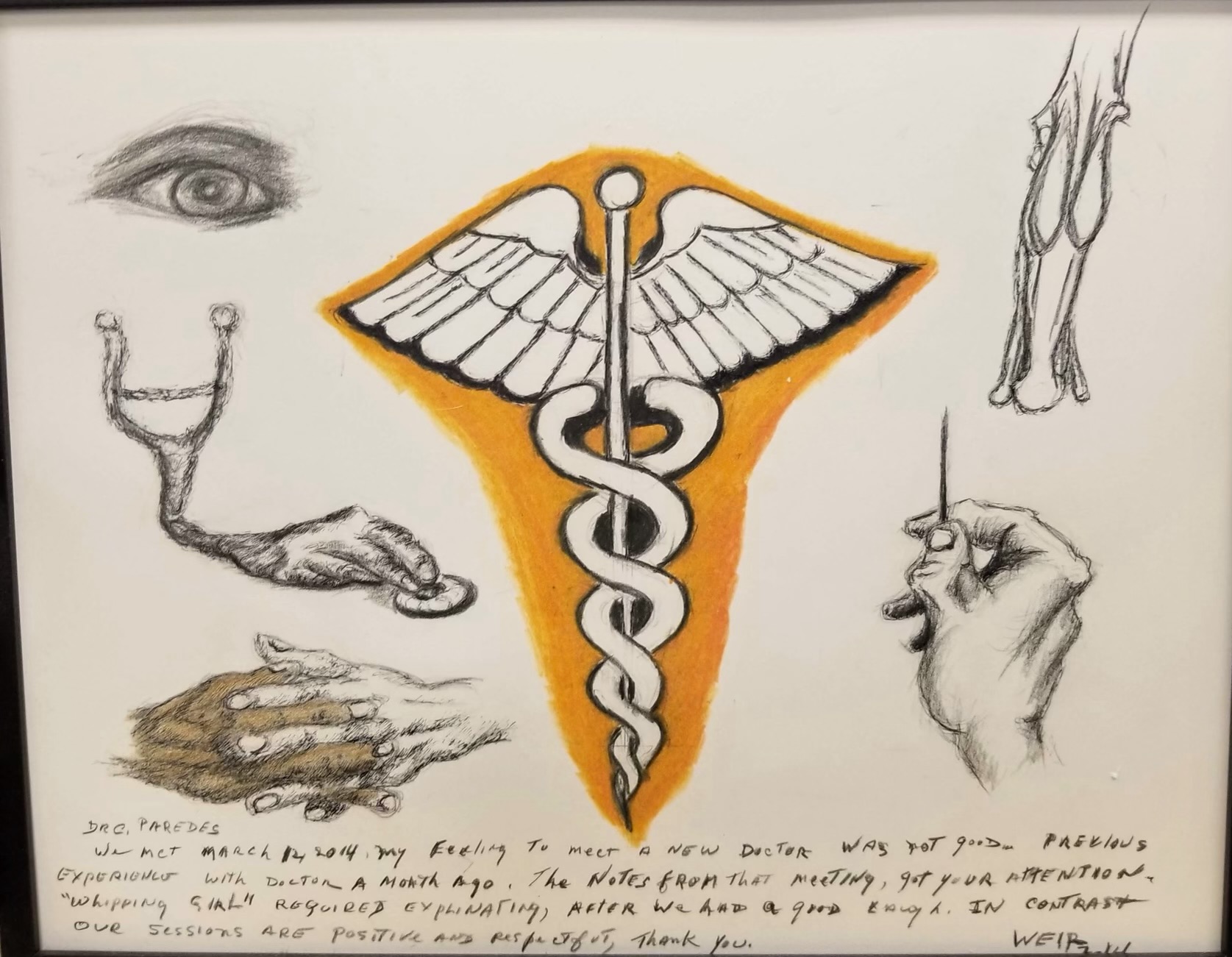
Art by Walter J. Weir
As time went on, our relationship developed. Each time I visited, I would always compliment one or another piece of his art, and during one visit he said if I liked a piece, I should take one as a gift. Instead, I challenged him, which he enjoyed as an artist, to create a piece that symbolized our relationship. So, this man—who was in his late 70s and suffering from diabetic retinopathy, so, poor vision, and neuropathy in his hands and legs—created this drawing for me, even though he couldn’t feel the pencil in his hand. When he gave me the drawing, he explained the meaning behind each element in it:
- The eye is for the way I looked at him and saw him as a whole person, as a human.
- The stethoscope with a hand is for the way I examined him.
- The two hands of different colors represented him and me working to come up with a care plan together.
- The leg with the brace was because, like the brace that supports his leg, I supported him and his medical conditions.
- The needle with the arthritic hand illustrated his struggles with diabetes and arthritis.
- And the caduceus was for my being a medical doctor whom he could trust.
Finally, he wrote me a personal note expressing his feelings about our relationship. All of that really affirmed to me that this path my mother started me on—to make a difference in people’s lives and touch them—was the right one for me. Home-based primary care is a way to make people human again, to educate and help them take control of their health by having a genuine relationship with their physician.
HCCInsights: How does your mom feel about what you’re doing these days?
Dr. Paredes: Oh, she’s proud for sure—she brags, “That’s my son, the doctor. He does geriatrics.” But she has a pretty great story herself, coming from poverty in the Philippines, studying by candlelight, becoming an OB-GYN there, and then having to start all over in the U.S. to get to where she is now. She’s very much one of those hardcore, old-school doctors. Her work ethic is impeccable and very clinically sound.
HCCInsights: How would you describe Northwell Health as an organization?
Dr. Paredes: Northwell Health is a large health system, but it’s very community-driven and patient-centered. Northwell has 21 hospitals, 850 outpatient facilities and more than 12,000 affiliated physicians, which makes it the largest health system in New York. We’re involved in every aspect of the community—from home-based primary care to amazing cardiothoracic surgery—and, as an organization, Northwell is very supportive of its clinicians and their goals in caring for patients.
Read the PDF version of this story here.